How To Pass The Multi-Specialty Recruitment Assessment (MSRA)
All eligible Anaesthetics applicants will be invited to attend the Multi-Specialty Recruitment Assessment (MSRA).
The MSRA is a computer-based assessment, delivered in partnership with Work Psychology Group and Pearson VUE, which has been designed to assess some of the essential competences outlined in the Person Specification and is based around clinical scenarios. The MSRA has two component parts - a Professional Dilemmas (PD) paper and a Clinical Problem Solving (CPS) paper. The MSRA is delivered as a single exam.
The MSRA will be delivered at Pearson VUE testing centres with remote testing provisions in place for those who are isolating/shielding due to COVID-19 or depending on their geographical location, local or national COVID-19 lockdown measures preventing access to a testing centre. The testing window is Thursday 28th January – Friday 12th February 2021.
The MSRA will be used to determine invitation to online interview where the number of eligible applicants exceeds interview capacity. There is no maximum achievable score. This will be known as shortlisting hereafter.
Your MSRA score will contribute 15% towards your total selection score. The PD and CPS elements will be weighted equally at 7.5%. MSRA scores are scaled for each specialty, so that they can be combined with the rest of the selection process, and appropriately weighted, as intended.
The General Practice NRO (GPNRO) lead the delivery of the MSRA on behalf of all participating specialties and has developed a separate guide which provides applicants with information about the whole MSRA process (e.g. registering to sit the test, centre locations, format of the assessment, etc.)
All applicants are expected to read this document in full to develop an understanding of this stage of the recruitment process and what is expected of applicants; it is available from the ANRO website.
Sitting The MSRA For CT1 Anaesthetics/ACCS Anaesthetics
All applicants who apply to Anaesthetics/ACCS Anaesthetics CT1 are required to sit the MSRA.
Important: The MSRA will be delivered at Pearson VUE test centres and a remote testing provisions will in place, as a reasonable adjustment, for those who are isolating/shielding in line government or public health guidance due to COVID-19 or, depending on their geographical location, where local or national COVID-19 lockdown measures prevent access to a testing centre due to site closures or travel restrictions.
The MSRA Structure
There are two component parts to the MSRA - a Professional Dilemmas (PD) paper and a Clinical Problem Solving (CPS) paper. The length of each paper is as follows:
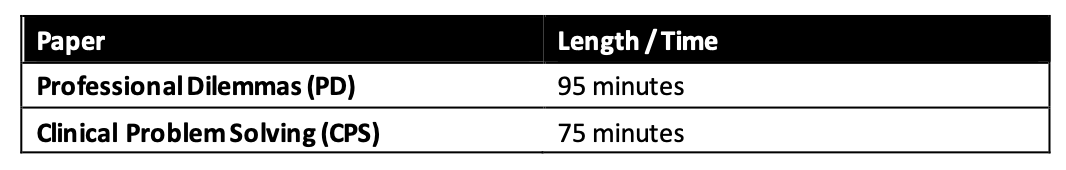
The MSRA is delivered as a single exam. The two papers are independently timed and the time remaining in each paper is denoted by an onscreen countdown timer.
On completion of the Professional Dilemmas paper, there will be a 5-minute scheduled break before the Clinical Problem-Solving paper commences. In instances where a break of longer than 5 minutes is take the excess time will be automatically taken off the available time for the Clinical Problem- Solving paper when you commence the paper.
The structure of both papers, including the question types, the competency domains being assessed and the scoring process is detailed in full in the MSRA Test Blueprint & Information document; you are strongly advised to read this document. Sample and practice questions for both of the papers are available from the GPNRO Resource Bank.
In addition to the MSRA Test Blueprint & Information document and sample questions , Pearson VUE offer a generic demo to aid you in familiarising yourself with the controls and screen layouts in advance of the test. This demo can be accessed via https://home.pearsonvue.com/nro.
Both parts of the MSRA are designed to assess those with a foundation level of competence.
The PD paper provides scenarios in the workplace for applicants to demonstrate their judgement about the most appropriate behaviours in that context. The PD content directly relates to the Generic Professional Capabilities framework outlined by the GMC which are required capabilities of all doctors.
The CPS is a test of how candidates can apply their clinical knowledge to make clinical decisions and is based on the Foundation Programme curriculum.
Therefore, the MSRA is relevant and fair for doctors applying for any medical specialty. For more information about why and how the MSRA is used for the specialty to which you are applying, please refer to the specialty recruitment website.
The Professional Dilemmas (PD) Paper
The PD paper is a Situational Judgement Test (SJT). This part of the assessment focuses on a candidate’s approach to working as a doctor. Specifically, the paper measures one’s understanding of situations that arise for doctors in the NHS (during a Foundation Placement) and judgement in choosing more or less appropriate responses to that situation, based on an understanding of what is more or less important. It focuses on appropriate behaviours when interacting with patients and colleagues and in managing one’s work. It does not require specific knowledge of experience in specialty training but does assume general familiarity with typical primary/secondary care work.
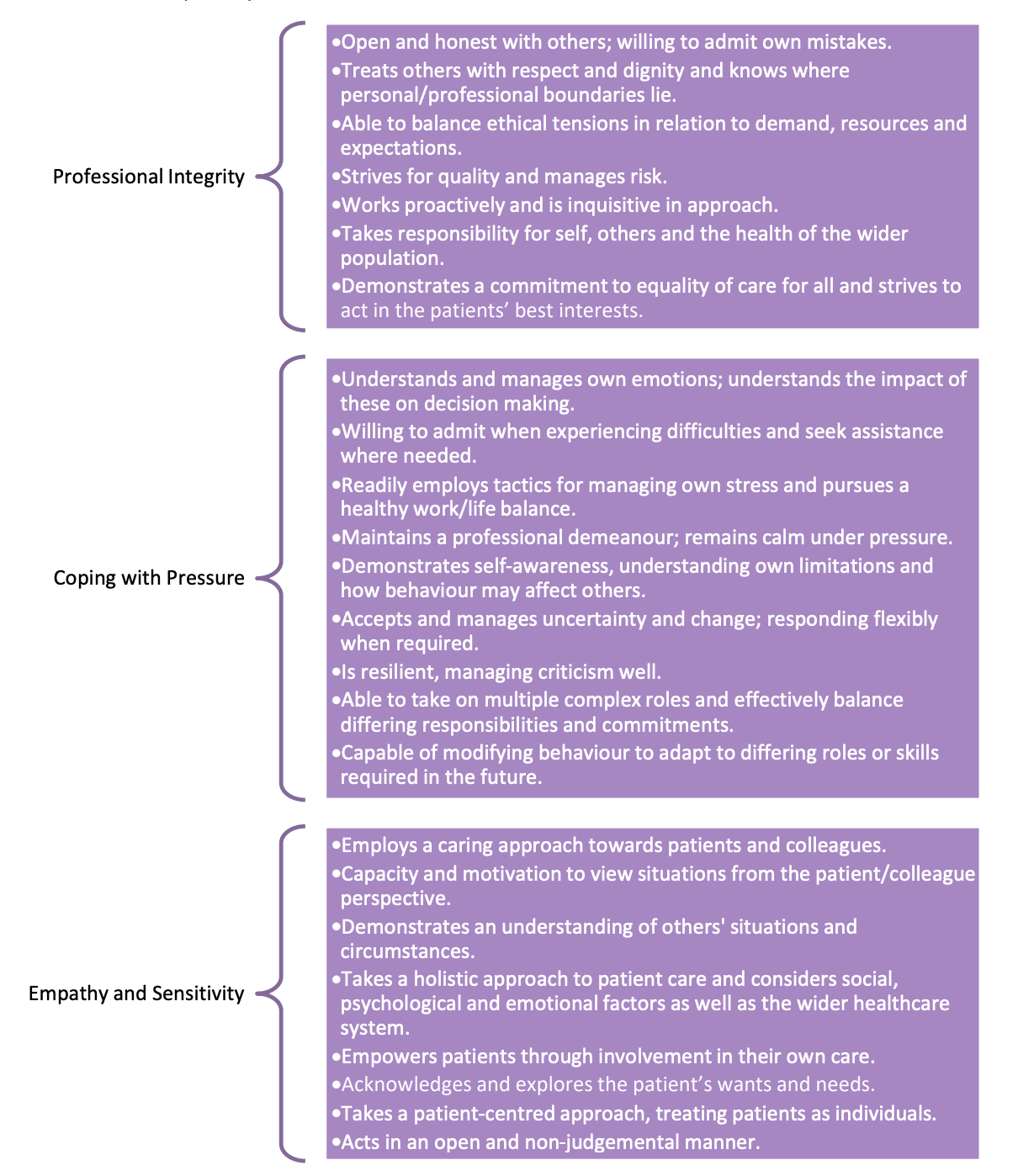
The test covers three core domains:
▪ Professional integrity
▪ Coping with pressure
▪ Empathy and sensitivity
The PD paper consists of 50 items and there are 95 minutes in which to complete the test. Only 42 items account towards the final score, as 8 of the items in each test paper are being tested (‘piloted’) before use.
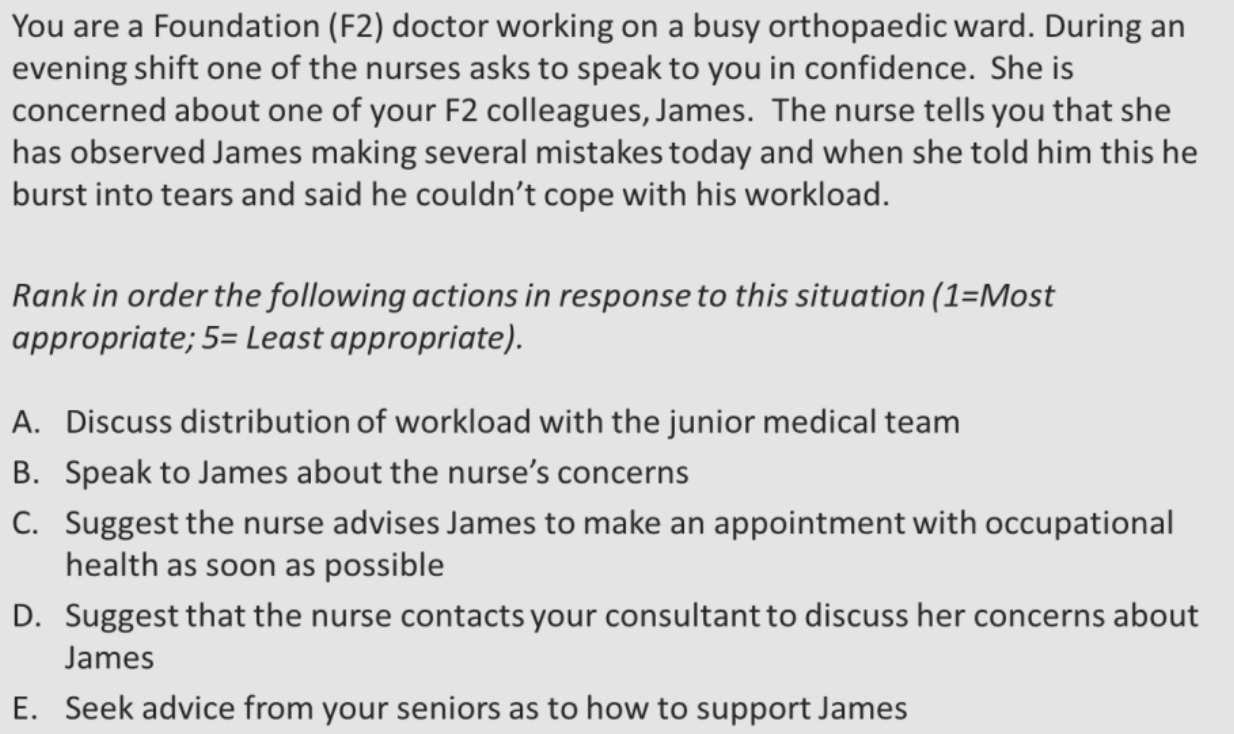
As the PD test is a measure of aptitude for entry to specialty training, it is set within the context of the Foundation Programme, with the candidate assuming the role of an F2 doctor. Although the candidate is asked to assume the role of a F2 doctor, each scenario is reviewed by Subject Matter Experts (SMEs) to ensure that the scenario does not contain any knowledge of procedures or policies that would only be applicable in certain localities or that are very UK-specific, as this would disadvantage certain candidates (i.e. International Medical Graduates).
In order to ensure that the PD paper is relevant to candidates applying to any specialty, and to increase the overall face validity of the test, the blueprint also requires that items are based within a range of contexts and rotations that a Foundation Doctor would realistically find themselves in. Therefore, there is a mixture of items based in hospital settings (across a variety of wards/placements), general practice, out-of-hours clinics, as well as a few based outside of a medical context (where relevant).
Even where a setting is specified in the question, this has only been chosen to provide a context, but the judgement required to answer the question is not specific to that setting.
The PD test covers three core competencies. Behavioural indicators linked to each
competency are outlined below:
The Professional Dilemmas (PD) Paper Question Types
There are 50 scenarios in the PD paper. Around half of the questions are ‘rank options in order’ and the other half are ‘multiple choice’. There is no negative marking, so you should attempt to answer all questions.
Responses to scenarios are usually actions taken to address the situation. Response options will be realistic and the ‘best response’ will always be included. For scenarios where the candidate is asked to consider the appropriateness of actions (whether ranking or multiple choice), there will be a mixture of good, acceptable and poor responses to the situation, as judged by SMEs. Completely implausible responses are not included as options.
Part 1 – Ranking: Candidates are asked to judge the appropriateness of four or five
independent actions, i.e. ‘Rank in order the following actions in response to this situation (1= Most appropriate; 5= Least appropriate)’. These scenarios require the candidate to think about the appropriateness of each of the different options presented. For these scenarios the actions are discrete actions and should not be thought of as
chronological. An example is presented below:
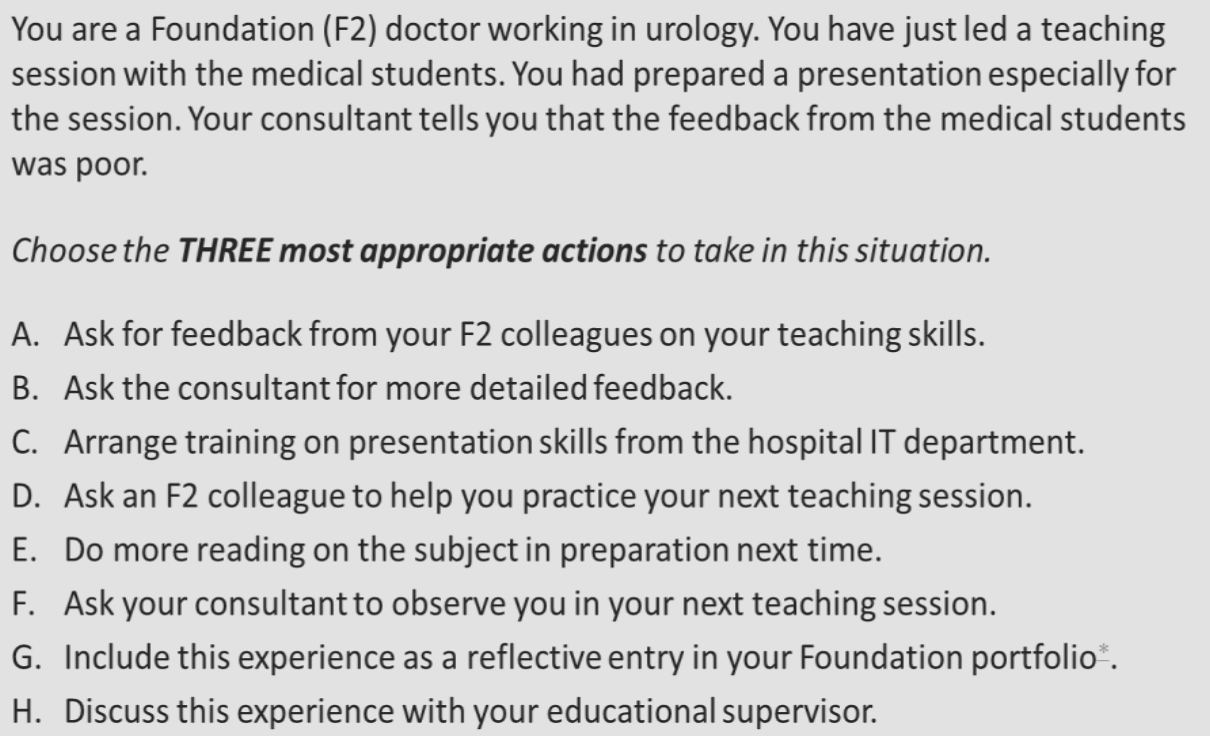
Part 2 – Multiple Choice: Candidates are asked to select three most appropriate actions to take in combination, out of a total of eight plausible actions, i.e. ‘Select the THREE most appropriate actions to take in this situation’. These scenarios require the candidate to think about the appropriateness of each of the options presented. The three most appropriate actions taken together should fully resolve the situation. An example is presented below:
The Clinical Problem Solving (CPS) Paper
In the CPS part of the assessment, candidates are presented with clinical scenarios that require them to exercise judgement and problem solving skills to determine appropriate diagnosis and management of patients. This is not a test of knowledge per se, but rather one’s ability to apply it appropriately. The items are based on Foundation-level clinical practice, and test higher level knowledge synthesis of medical knowledge.
The CPS paper consists of 97 questions and there are 75 minutes in which to complete the test. Only 86 items account towards the final score, as 11 of the items in each test paper are being tested (‘piloted’) before use.
The Clinical Problem Solving (CPS) paper is an assessment which measures the candidate’s ability to apply their clinical knowledge in and make clinical decisions in everyday practice. The scenarios are based on Foundation-level clinical practice, and are testing a candidate’s ability to synthesise and apply medical knowledge (not just their recall of knowledge).
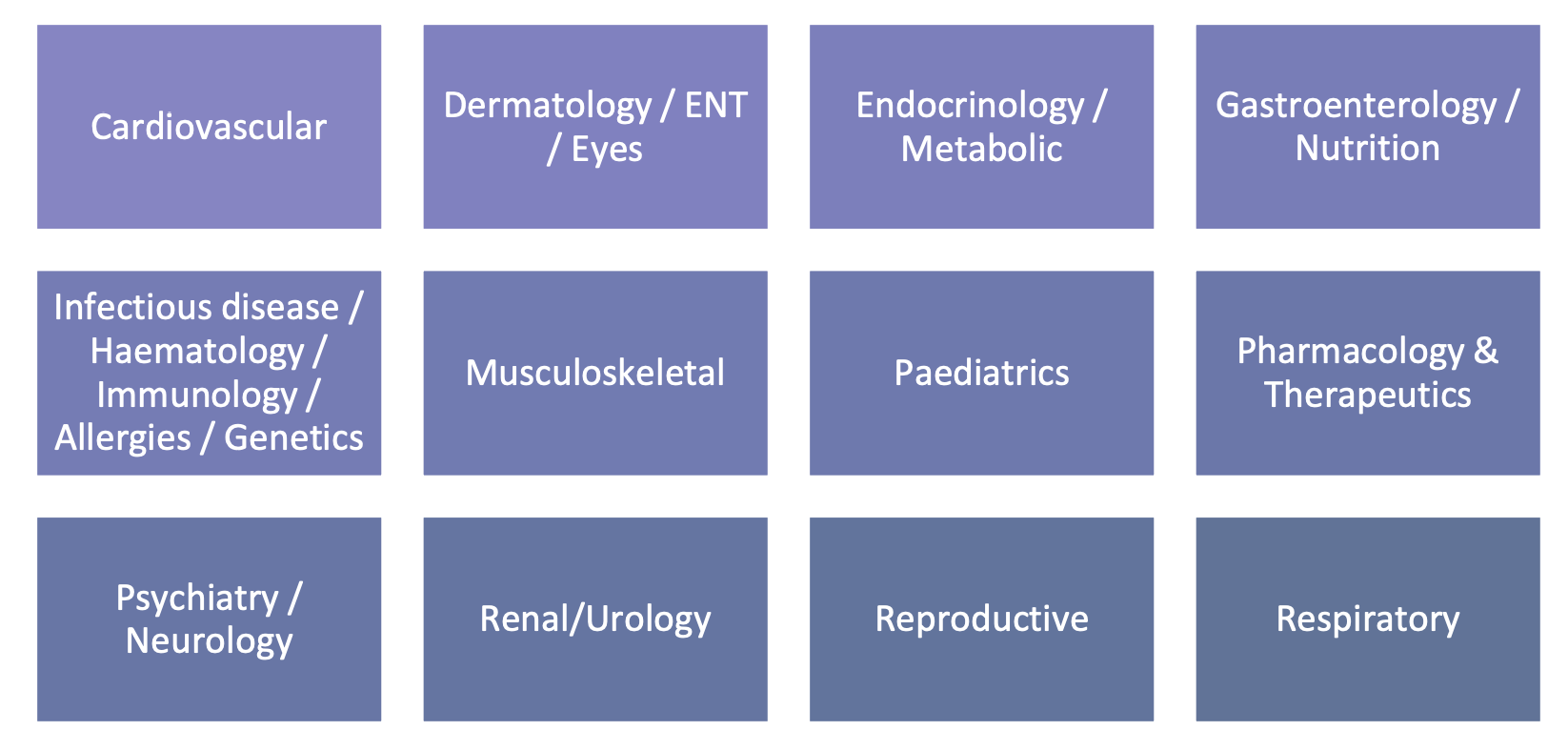
CPS items are based in 12 clinical topic areas relevant to general medicine and each test paper includes a balance of scenarios which cover all 12 topics. The topics covered include:
The test covers five core domains / competencies. The competencies and their definitions are provided below:
1) Investigation: specific investigations that are carried out in order to obtain a more conclusive diagnosis, or rule out possible causes of illness/injury
2) Diagnosis: identification of a condition, disease or injury made by evaluating the symptoms and signs presented by a patient
3) Emergency: potential serious illness requiring an immediate response (recognising patient risk based on suggested factors)
4) Prescribing: advising, authorising or reviewing the use of medicine/drugs as part of a patient's clinical management plan
5) Management (non-Prescribing): advising, authorising or reviewing the use of other forms/methods of treatment (not medicinal/drug-related) as part of a patient's clinical management plan
The Clinical Problem Solving (CPS) Paper Question Types
There are 86 items in the CPS paper. Around half of the items are Extended Matching Questions (EMQ) and the other half are Single Best Answers (SBA). EMQs refer to multiple clinical scenarios that are linked to the same set of response options.
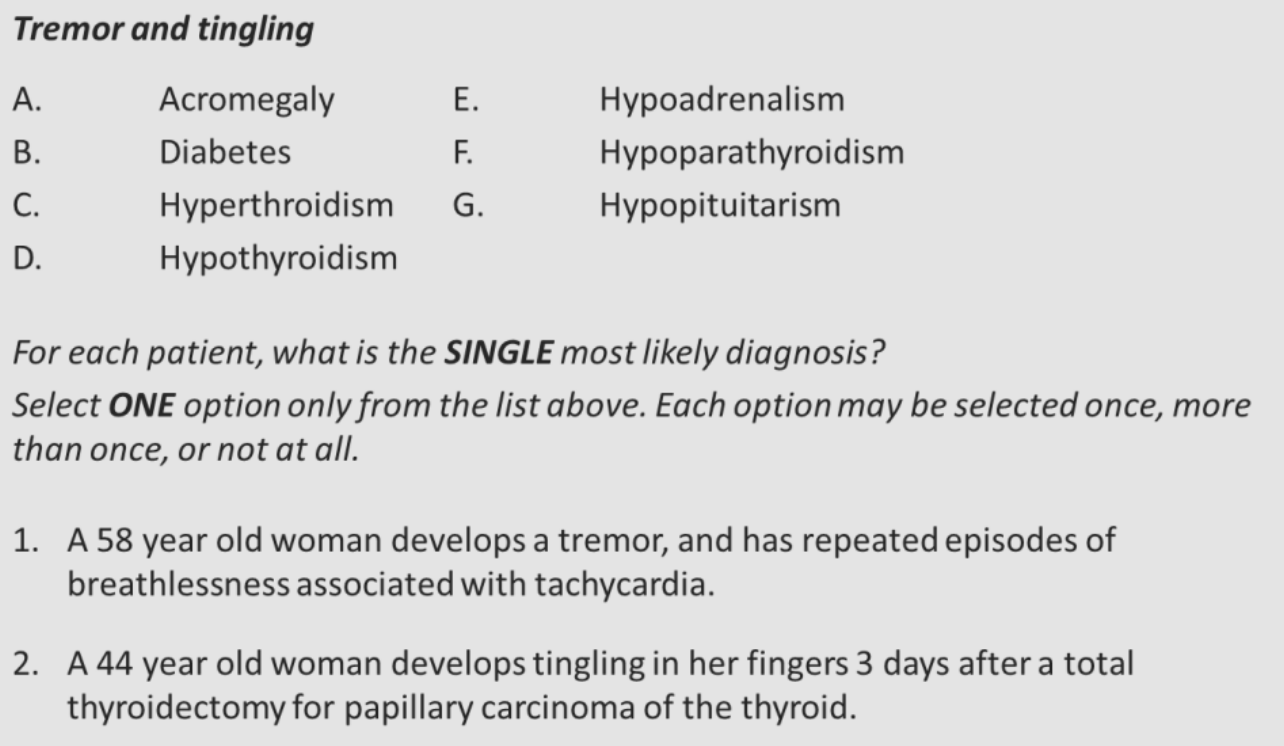
Extended Matching Question (EMQ): Candidates are presented with a list of 7-10 plausible response options and multiple, separate questions linked to this response set.
Candidates will need to select the most appropriate or likely answer for each clinical presentation, i.e. ‘For each patient, please select the most appropriate drug to prescribe.’. Each response option can be selected once, more than once or not at all when responding to the set of cases. An example is presented below.
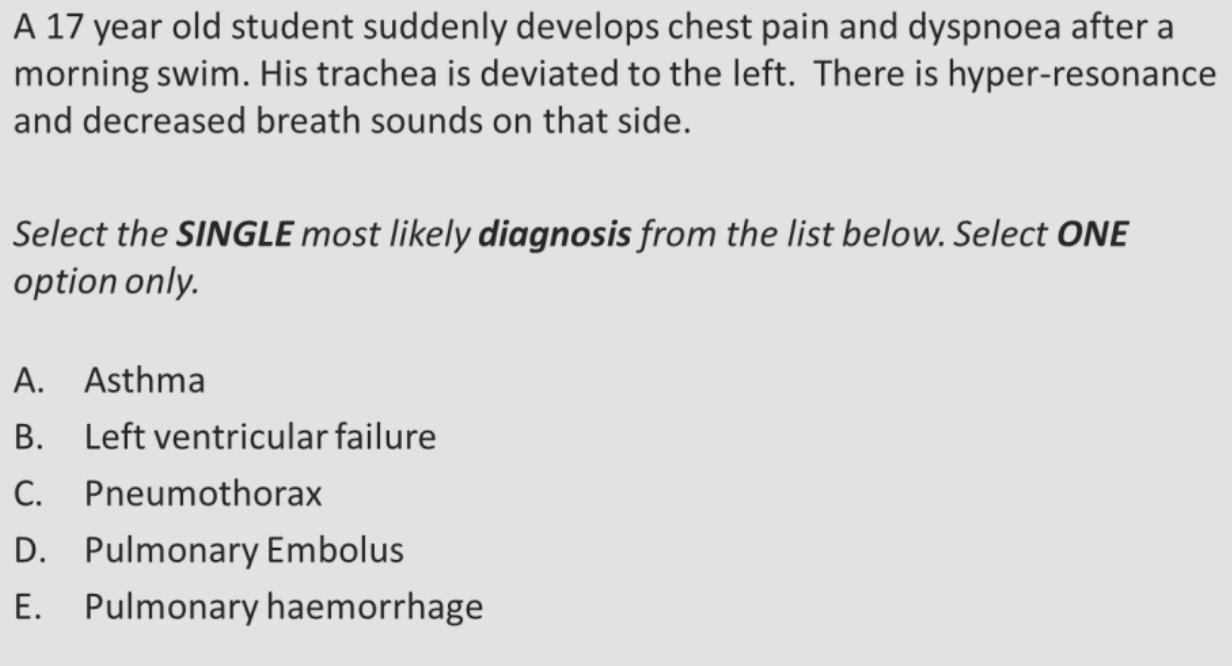
Single Best Answer (SBA): Candidates are asked to select the single most appropriate or likely answer out of 5- 8 plausible responses for one clinical presentation, i.e. ‘Select the SINGLE most appropriate diagnosis from the list below’. An example is below.
Registering For The MSRA
Once the application window has closed, you will receive a message from the ANRO asking you to register with Pearson VUE using very specific account credentials associated with your new Oriel 2 account. If you have applied to other specialties, you may receive multiple messages containing the same credentials from each. In this instance, you only need to register once.
Accounts previously created for the MSRA with credentials associated with the older version of Oriel will no longer be valid from this recruitment year.
Failure to register will result you being unable to sit the MSRA and your Anaesthetics/ACCS Anaesthetics CT1 application will be withdrawn.
It is important to remember that the registration correspondence is not an invitation to attend the MSRA; on completion of registration, your account will correctly state you do not have any pre- approved exams at this time meaning you will not be able to book an appointment.
Following the successful completion of the registration process, applicants will be able to sign into their new or existing Pearson VUE accounts by visiting https://home.pearsonvue.com/nro.
Applicants who are unable to recall their login credentials can retrieve or reset this information by using the forgot my username / password links available on the sign-in page.
Applicants who continue to experience difficulties accessing their account are advised to direct their queries to the Pearson VUE customer services team at [email protected]. When contacting customer services, please ensure the following information is provided:
• Your Pearson VUE Application Number (i.e. your 12-digit Oriel Exam ID)
• Your, full name, as registered on the Pearson VUE account
• Your email address, as registered on the Pearson VUE account
• Your postal address, as registered on the Pearson VUE account
Invitation To The MSRA
All applicants who have been assessed as demonstrating evidence of eligibility as outlined in the Longlisting section of the Anaesthetics/ACCS Anaesthetics CT1 Applicant Guidance will be invited to sit the MSRA. If you are invited, you will be required to book an appointment and undertake the MSRA; failure to do so will result in your application(s) not progressing further.
All invitations will be for the delivery of the MSRA in Pearson VUE test centres. Once invitations have been received, applicants who are isolating/shielding due to COVID-19 or are prevented from accessing a test centre due to local or national COVID-19 lockdown measures, will have the opportunity to request sitting the MSRA remotely by exception. The MSRA team will approve requests on a case by case basis. Remote testing is not available to applicants for any non-COVID-19 related issues.
MSRA Scoring
The MSRA scores will be used to rank applicants for shortlisting purposes, based on the maximum interview capacity. There is no maximum achievable score.
The MSRA score will contribute 15% towards your total Anaesthetics/ACCS Anaesthetics CT1 Selection Score. The PD and CPS elements will be weighted equally (i.e. each will be weighted at 7.5%). MSRA scores are scaled for each specialty, so that they can be combined with the rest of the selection process, and appropriately weighted, as intended.
MSRA Candidate Tips
A generic tutorial is available to allow you to familiarise yourself with the controls and screen layouts in advance – see Pearson VUE or Oriel for details.
A glossary of frequently used terms and a list of abbreviations is available for reference throughout the exam. This is particularly useful for those less familiar with the UK medical system.
Papers are NOT negatively marked so make sure you answer all the questions. A wrong answer can score more marks than a missed question.
Read the instructions and questions carefully. There may be times when you would like more information to answer questions; you need to give your best answer using the information provided in the question.
For the SJT it is important to bear in mind that answers are marked against a predetermined key, based on a near-miss approach. Your performance on the test as a whole will be used to determine your level of situational judgement.
Read the example questions provided carefully. If you feel you would benefit from revisiting some areas of knowledge or practice in order to be better able to show your capability, then you should do this before the assessment.
The MSRA is coordinated by the GPRO and further samples can be found here.